Automate. Analyze. Accelerate Growth for Health Insurance.
Fintary helps health insurance companies and brokerages automate complex reconciliation, uncover new revenue, and empower producers with real-time insights — all on one intelligent platform.

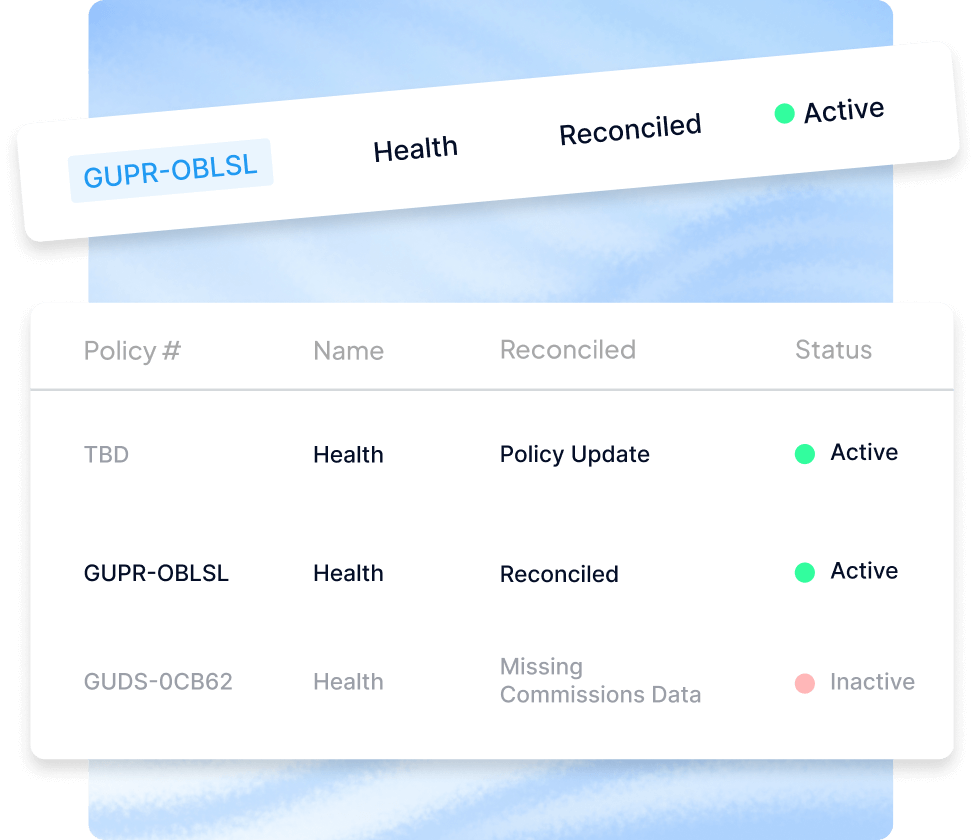
Process complex group statements automatically with AI

Fixed-rate reconciliation without manual calculations

Instant discrepancy detection and reporting